You are here
September 24, 2019
Two commonly used drugs for uveitis perform equally well
At a Glance
- The drug methotrexate performed as well as the more expensive mycophenolate mofetil for treating uveitis, a form of eye inflammation.
- The findings provide new guidance for treating uveitis.

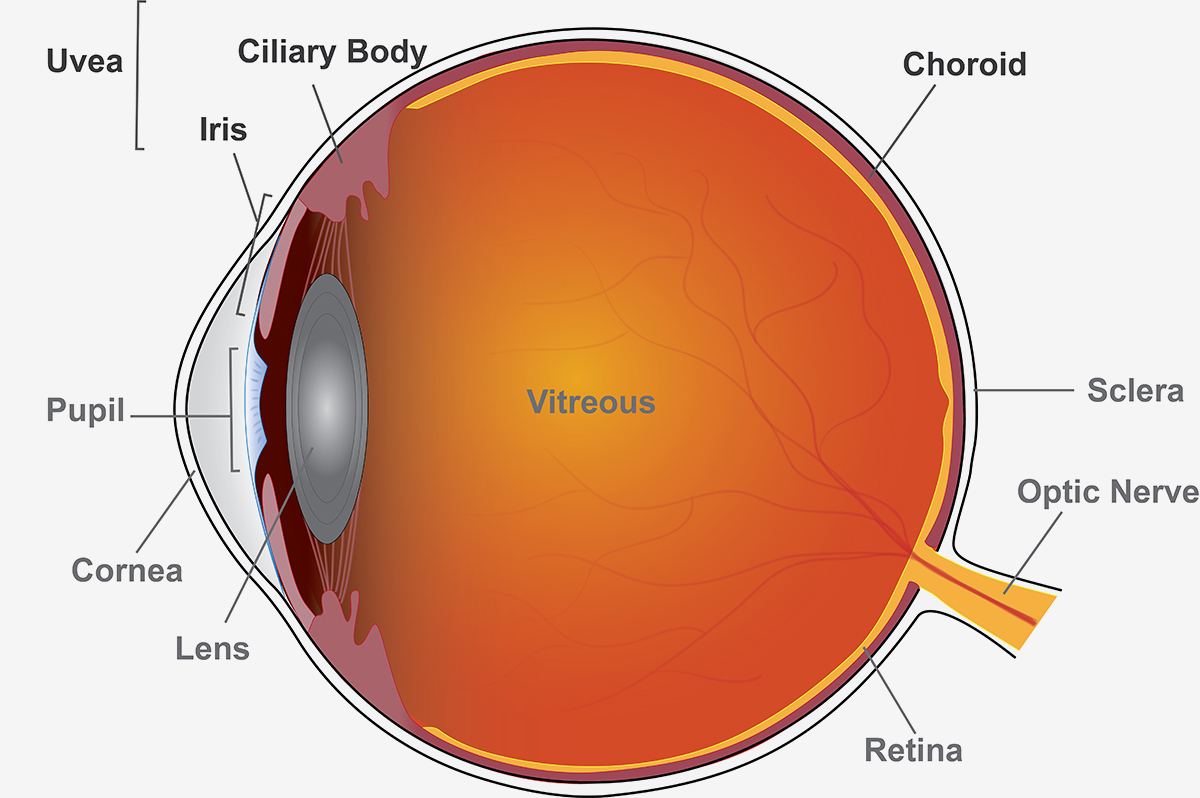
Uveitis is an eye disease responsible for up to 1 of every 6 blindness cases in the U.S. It’s caused by inflammation of the eye’s middle layer of tissue called the uvea. Early signs of uveitis include eye pain, redness, sensitivity to light, blurry vision, and floaters (seeing specks or shadows).
Uveitis can be caused by a misguided attack from the body’s own immune system. It can also result from infections or tumors, bruises to the eye, or toxins.
Noninfectious uveitis is often first treated with oral corticosteroids like prednisone to control inflammation. But being on high doses for a long time can have serious side effects, so patients are soon reduced to a low dose and switched to other drugs. Methotrexate and mycophenolate mofetil are commonly used medications. They work by suppressing the immune system.
A research team led by Dr. Nisha Acharya of the University of California, San Francisco, set out to determine which of these uveitis drugs was more effective when moving beyond corticosteroid treatment. The international study was funded by NIH’s National Eye Institute. Results were published on September 10, 2019, in JAMA.
The team randomly assigned 216 patients with uveitis to receive methotrexate or mycophenolate. The patients had intermediate and posterior uveitis, which affects the middle and back of the uvea, or panuveitis, which affects all layers. Over six months, the participants reduced their prednisone to 7.5 milligrams a day or less and received either three grams of mycophenolate daily or 25 milligrams of methotrexate weekly.
To assess the treatments, the researchers performed eye exams and imaged the front and back parts of the eye. At six months, both medications were similarly effective: 67% of participants in the methotrexate group and 57% in the mycophenolate group had control of their inflammation and successfully reduced corticosteroids.
Patients who did not respond had the option to switch treatments. At one year, 69% of participants who had switched from mycophenolate to methotrexate had treatment success. Only 35% of those participants who switched from methotrexate to mycophenolate had control over inflammation.
Notably, the researchers found that methotrexate was more effective than mycophenolate for treating the most severe forms of uveitis—posterior uveitis and panuveitis. At six months, 74% in the methotrexate group had control over their disease versus 55% in the mycophenolate group. Among patients with intermediate uveitis, the difference between groups wasn’t significant.
Patients in the study tolerated both drugs equally well. Both can cause fatigue, nausea, and headaches. Serious side effects, related to liver function, were rare.
“Based on this head-to-head clinical trial, methotrexate is as good as or better than mycophenolate for treating uveitis. That’s important because the prior literature and a survey on treatment preferences suggests most clinicians believe the opposite. Now we have a randomized trial to provide guidance on treatment,” Acharya says. “Additionally, there’s a cost difference in the U.S., where mycophenolate to control uveitis is over five times more expensive.”
Related Links
- Novel Gene-Editing Method Improves Vision in Blind Rats
- “Intelligent” Injection Device Targets Tissues
- Regenerating Retinal Cells in Mice
- Refining Supplements for a Blinding Eye Disease
- Comparing Treatments for Age-Related Eye Disease
- Facts About Uveitis
- Learn About Eye Health
References: Effect of Corticosteroid-Sparing Treatment With Mycophenolate Mofetil vs Methotrexate on Inflammation in Patients With Uveitis: A Randomized Clinical Trial. Rathinam SR, Gonzales JA, Thundikandy R, Kanakath A, Murugan SB, Vedhanayaki R, Lim LL, Suhler EB, Al-Dhibi HA, Doan T, Keenan JD, Rao MM, Ebert CD, Nguyen HH, Kim E, Porco TC, Acharya NR; FAST Research Group. JAMA. 2019 Sep 10;322(10):936-945. doi: 10.1001/jama.2019.12618. PMID: 31503307.
Funding: NIH’s National Eye Institute; Research to Prevent Blindness; That Man May See Foundation.